
Autism spectrum disorders (ASDS)
Autism and autism spectrum disorders (ASDs) are complex, severe, heterogeneous neuro-developmental multifactorial pathologies originating from the interaction of several genes with environmental and immunological factors.
Despite much progress in our understanding of the associated immunobiology of autism, the pathogenesis of autism, as well as the defined molecular mechanisms, remain unclear. The dramatic increase in prevalence (one in 42 boys and one in 189 girls) [CDC data, Baio 2014] underscores the urgent need for specific biomarkers to facilitate the early diagnosis and treatment of ASDs. The precise mechanisms of immunological dysregulations are incompletely understood, however progress is allowing more insight into the complex imbalances associated with ASDs. Autism is now accepted to be commonly associated with significant immunological abnormalities ranging from the gastrointestinal associated immune system to the microglial innate immune cells of the central nervous system.
Biomarkers for autism
Immune dysfunction in autism: a pathway to treatment
Autism is a complex and clinically heterogeneous disorder with a spectrum of symptoms. Published findings have identified widespread changes in the immune systems of children with autism, at both systemic and cellular levels. Together, these reports suggest that autism may in fact be a systemic disorder with connections to abnormal immune responses. Such immune system dysfunction may represent novel targets for treatment.” (Careaga et al. Neurotherapeutics 2010).


Cytokine imbalances in autism spectrum disorders (ASD)
There are many reports of cytokine imbalances in autism spectrum disorders (ASD). These imbalances may have a pathogenic role, or they may be markers of underlying genetic and environmental influences. Cytokines act primarily as mediators of immunological activity but they also have significant interactions with the nervous system. Cytokine profiles change dramatically in the face of infection, disease, and toxic exposures. Ashwood et al. (Brain Behav Immun. 2011) reported significant increases in the plasma levels of a number of cytokines, including IL-1β, IL-6, IL-8 and IL-12p40 in the subjects with ASD when compared to controls.
Additionally, Suzuki et al. (PLoS One 2011) reported that the plasma concentrations of IL-1β, IL-1RA, IL-5, IL-8, IL-12(p70), IL-13, IL-17 and GRO-α were significantly higher in subjects with ASD compared with the corresponding values of matched controls. Finally, Okada et al. (Prog Neuropsychopharmacol Biol Psychiatry 2007) and Ashwood et al. (J Neuroimmunol. 2008 ) independently reported thet serum levels of transforming growth factor-beta1 (TGFb1) were decreased in patients with autism. Furthermore, lower TGFb1 levels were associated with lower adaptive behaviors and worse behavioral symptoms, suggesting that immune responses in autism may be inappropriately regulated due to reductions in TGFb1.
The association between tick-borne infections, lyme borreliosis and asds
An association between Lyme disease (LYD) and other tick-borne infections (TBI) during fetal development and in infancy with autism, autism spectrum disorders (ASD) and autistic symptoms has been noted by numerous clinicians and parents. Bransfield et al. wrote in 2008 a review paper (Med Hypotheses 2008; 70:967-74) to collate information from conference presentations on this issue with other sources that further address this association. They indicated that the preliminary data suggests Borreliosis may be a contributor in 20– 30% of ASD, and pathogenic Mycoplasma may be a contributor in 58%.
Kuhn et al. (Med Hypotheses 2012; 78:606-15) suggested that long-term antibiotic therapy might be an effective treatment for children co-morbid with Lyme disease and autism spectrum disorder.

Offutt A, Breitschwerdt EB. Case report: Substantial improvement of autism spectrum disorder in a child with learning disabilities in conjunction with treatment for poly-microbial vector borne infections. Front Psychiatry. 2023 Aug 18

Prostaglandin E2 (PGE2) has been found to be significantly higher in autistic patients, recording an increase of 91.15%
“Prostaglandin E2 (PGE2) is a compound derived from membrane phospholipids and an important mediator of synaptic plasticity, pain response, sleep/ awake cycle and is believed to be associated with inflammation in the brain. PGE2 was significantly higher in autistic patients, recording an increase of 91.15% (El-Ansary & Al-Ayadhi ; Lipids Health Dis. 2012;11:160). Elevated prostaglandins could be related to the recent record of Rossignol and Frye (Mol Psychiatry 2012;17:389–401) that immune dysregulation/ inflammation are the first etiological factor of autism.
It is well known that autism could be associated with viral infections, which cause an up regulation in prostaglandins that then mediate fever production. This suggestion could support the elevated inflammatory cytokines in the plasma and brains of autistic patients. The significant elevation of PGE2 in autistic patients compared to age-matched control participants could be related to glutamate exitotoxicity, lower GABA and autistic amygdala lesion as factor related to the social abnormalities in autism.
This study could help to list PGE2 among predictive biomarkers usually used to predict outcome to a specific treatment. This study could help to suggest omega-3 Long Chain Polyunsaturated Fatty Acids supplementation as a strategy for the early intervention to ameliorate pro-inflammation and oxidative stress related symptoms in autism.” (From: El-Ansary A, Al-Ayadhi L. Lipids Health Dis. 2012;11:160)
Nagalase activity in patients with autism : substantially higher levels than the expected healthy ranges
“In this first report of Nagalase activity in patients with autism, it appears that most individuals have substantially higher levels than the expected healthy ranges. Although Nagalase is a nonspecific marker of immune dysregulation, its observed levels in autism may have both etiological and therapeutic significance. Importantly, this is also the first report of reduction of Nagalase activity in an autism population with GcMAF injections.
Regardless of any immediate clinical improvement, the reduction of Nagalase to more desirable levels is of potential benefit to these patients, since Nagalase is known to impair immune defenses.” ( From: Bradstreet et al. Journal: Autism Insights 2012; 4: 31-38).
Nagalase is a component of viral hemagglutinin and is released by the action of trypsin on hemagglutinin. Since hemagglutinin is a common glycan-binding lectin of many viruses (including influenza, paramyxoviruses and polyomaviruses), several viruses may individually or jointly contribute to hemagglutinin-derived Nagalase activity in the blood. In the absence of recent viral infection or malignancies, elevated Nagalase activity likely represents a marker of viral production of hemagglutinin protein being acted upon by inflammatory cell mediated trypsin activity; as such it may represent viral persistence, active transcription, and inflammation. Viral protein transcription is one potential mechanism of autoimmunity.
Beyond this, Nagalase is an enzyme that deglycosylates the Gc protein also known as vitamin D binding protein (VDBP), rendering it incapable of conversion to active GcMAF (Gc protein-derived Macrophage Activating Factor) and thereby preventing its regulation of macrophage activation. It is noteworthy that vitamin D deficiency, either in pregnancy or during postnatal development, is an apparent risk factor for autism. The impact of Nagalase on VDBP transportation of vitamin D is not known. However, vitamin D deficiency is a known risk factor for autoimmunity.
In this first report of Nagalase activity in patients with autism, it appears that most individuals have substantially higher levels than the expected healthy ranges. Although Nagalase is a nonspecific marker of immune dysregulation, its observed levels in autism may have both etiological and therapeutic significance. Importantly, this is also the first report of reduction of Nagalase activity in an autism population with GcMAF injections.


Cannabinoid receptors’ in autism
“Immune system dysregulation is well-recognized in autism and thought to be part of the etiology of this disorder. The endocannabinoid system is a key regulator of the immune system via the cannabinoid receptor type 2 (CB2R) which is highly expressed on macrophages and microglial cells. The mRNA level for cannabinoid receptor type 2 (CB2) was significantly increased in AD-PBMCs as compared to healthy subjects (mean ± SE of arbitrary units: 0.34 ± 0.03 vs. 0.23 ± 0.02 in autistic children and healthy subjects, respectively), whereas CB1 and fatty acid amide hydrolase mRNA levels were unchanged.
mRNA levels of N-acylphosphatidylethanolamine-hydrolyzing phospholipase D gene were slightly decreased The data from this study indicate CB2 receptor as potential therapeutic target for the pharmacological management of the autism care. GcMAF treatment was able to normalize the observed differences in dysregulated gene expression of the endocannabinoid system of the autism group.” (From : Siniscalco et al. J Autism Dev Disord. 2013; Siniscalco et al. J Neuroinflammation 2014).
Gastrointestinal status in children with autism correlate with autism severity
Alterations in the bowel flora are now believed to be contributing factors to many chronic diseases such as allergies, autoimmune and inflammatory disorders, ASDs, or degenerative diseases.
The intestinal microflora can be considered as a postnatally acquired organ, composed of a large diversity of bacterial cells that performs different functions for the host. The microflora plays a significant role in gut maturation, gut integrity, prevention of pathogenic and opportunistic bacterial colonization and modulates the immune system. It is also involved in vitamin synthesis, production of short chain fatty acids and metabolism of carcinogenic substances.
Although the intestinal flora is quite stable over time, a number of factors can disturb the normal balance leading to intestinal dysbiosis. Intestinal microflora can be altered by immune mechanisms of the host, redox state, adrenal function, intestinal pH, diet, aging, drugs, exogenous organisms and emotional stress. Intestinal dybiosis is seen in a number of chronic diseases such as Crohn’s disease, IBS, CFS and may be associated with developmental disorders such as autism and ADHD. Chronic Lyme disease can mimic every disease process including Chronic Fatigue Syndrome (Myalgic Encephalomyelitis) and Fibromyalgia. In fact, chronic Lyme is often called the “Great Imitator“.


Adams et al. (BMC Gastroenterology 2011) reported that gastrointestinal symptoms were strongly correlated with the severity of autism.
From four types of beneficial bacteria that were investigated, the children with autism had much lower levels of Bifidobacterium (-45%), slightly lower levels of Enterococcus (-16%), and much higher levels of Lactobacillus (+100%). Finegold et al. (Anaerobe 2012) reported that in the control children’s stools, Firmicutes accounted for 63.6% of the total flora but only 38-39% of the flora of autistic children’s stools. Bacteroidetes accounted for 30% of the stool flora in controls and for 51% in the flora of stools of autistic children. Actinobacteria made up 1.8% of stool flora of control children and between 0.4 and 0.7% of the flora of autistic children. Proteobacteria made up 0.5% of the flora of control children and between 2.3 and 3.1% of the flora of autistic children. In all cases, the flora of sibling controls was between the values of autism and control populations.
In summary, the fecal flora of autistic children was statistically significantly different from the fecal flora of healthy children.

Several reports have revealed a high prevalence of gastrointestinal symptoms, inflammation, and dysfunction in children with autism (reviewed by Horvath and Perman, Curr Gastroenterol Rep. 2002).
Mild to moderate degrees of inflammation were found in both the upper and lower intestinal tract. In children with ASD, the presence of GI dysfunction is often associated with increased irritability, tantrums, aggressive behavior, and sleep disturbances (reviewed by Critchfield et al., Gastroenterol Res Pract. 2011).
Evidence for mycoplasma spp., chlamydia and herpes virus coinfections in blood of adss patients
Nicolson et al. (J Neurosci Res. 2007;85(5):1143-8) examined the blood of 48 patients from central and southern California diagnosed with autistic spectrum disorders (ASD) and found that a large subset (28/48 or 58.3%) of patients showed evidence of Mycoplasma spp. infections compared with two of 45 (4.7%) age-matched control subjects (odds ratio = 13.8, P < 0.001). They also examined the prevalence of C. pneumoniae (4/48 or 8.3% positive, odds ratio = 5.6, P < 0.01) and human herpes virus-6 (HHV-6, 14/48 or 29.2%, odds ratio = 4.5, P < 0.01) coinfections in ASD patients. Control subjects also had low rates of C. pneumoniae (1/48 or 2.1%) and HHV-6 (4/48 or 8.3%) infections, and there were no coinfections in control subjects.
Their results indicate that a large subset of ASD patients shows evidence of bacterial and/or viral infections.
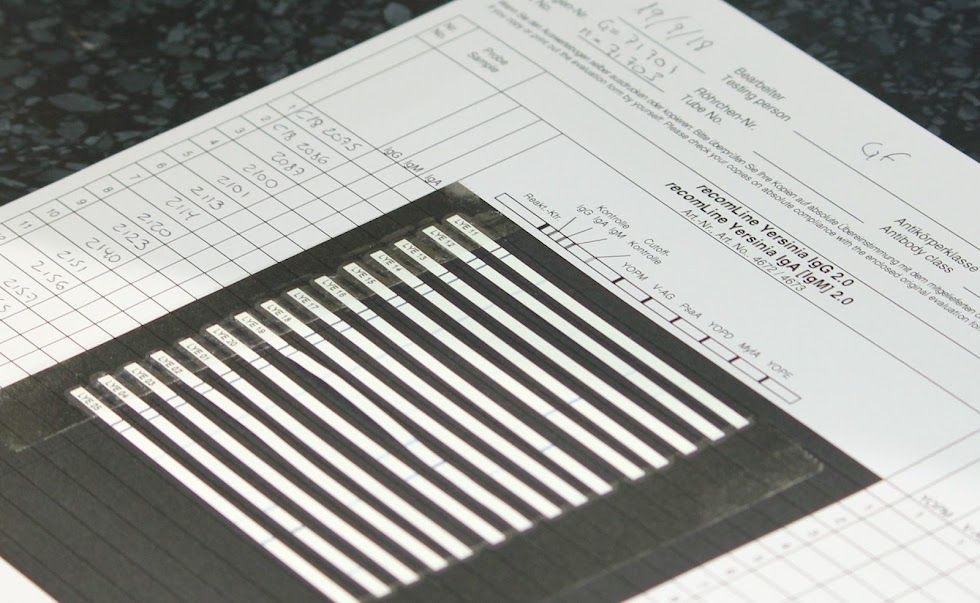
Yersinia and cmv infections in asd patients
Several autism-spectrum subgroups derive from intra-monocyte pathogens such as cytomegalovirus, human herpesvirus 6, and Yersinia enterocolitica. As reported by Blinstock (Med Hypotheses. 2001; 56(4):523-31), immune panels of many autism-spectrum children reveal signs of atypical infections and shifted cell counts. In conjunction with trait-related cerebral hypometabolism and hypoperfusion, these findings suggest a hypothesis: Several autism-spectrum subgroups derive from intra-monocyte pathogens such as measles virus, cytomegalovirus, human herpesvirus 6, and Yersinia enterocolitica.
Furthermore, with much inter-child variation, their effects manifest as diminished hematopoiesis, impaired peripheral immunity, and altered blood-brain barrier function often accompanied by demyelination. In some such children, one or more of these pathogens persists as a chronic-active, seemingly subclinical infection etiologically significant to the child’s autistic traits.
Within these subgroups, immune impairments and atypical infections may be treatable.



