Integrative approach for testing patients with autism spectrum disorders
The importance of assessing inflammation, infections and gastrointestinal disorders in autism spectrum disorders (asd) patients

TANJA MIJATOVIC, PHD R.E.D. LABS CSO & LAB MANAGER
Autism diagnosis



Immune dysfunction in autism
The importance of assessing inflammation, infections and gastrointestinal disorders in autism spectrum disorders (asd) patients

Inflammation and asd – well documented issue



Immune dysfunction in autism:
A pathway to treatment
“Autism is a complex and clinically heterogeneous disorder with a spectrum of symptoms. Published findings have identified widespread changes in the immune systems of children with autism, at both systemic and cellular levels. Together, these reports suggest that autism may in fact be a systemic disorder with connections to abnormal immune responses. Such immune system dysfunction may represent novel targets for treatment.” (Careaga et al. Neurotherapeutics 2010)
The autism diagnosis is suffering by the lack of a specific biomarker
Several biochemical pathways are associated with ASDs
Many testing panels are currently available for biomedical evaluation of multifactorial afflictions
Autism spectrum disorders are even more complex than most of multifactorial syndromes, needing thus a very specialized and personalized approach.

Immunity

Innate and acquired immunity

Immune dysfunction

Immune findings in ASD

HUGHUES ET AL. FRONT. CELL. NEUROSCI., 13 NOVEMBER 2018
A majority of children with autism exhibited low nk cell activity
Absolute count of CD56+ and CD57+ Natural killer cells
Vojdani et al (J Neuroimmunol. 2008) reported on low natural killer cell cytotoxic activity in autism. In their study, involving 1027 blood samples from autistic children obtained from ten clinics and compared the results to 113 healthy controls, 45% of the children with autism exhibited low NK cell activity.
CD57+/CD3- cells are a subset of NK cells. Their exact function, and what differentiates them from CD56+ NK cells, is not well understood. The absolute number of CD57+/CD3- cells is low in patients suffering from chronic Lyme disease (a disease that follows an infection by a bacteria called Borrelia). Patients with very low CD57 have significantly more co-infections and persistent immunologic defects than patients with higher counts. In patients that respond to antibiotic therapy, the number of cells come back to normal, hence this is a useful marker to follow the effect of a therapy.
Our study (Siniscalco et al, InVivo 2016) showed that on 107 autistic patients enrolled, 73 (68.2%) of them showed CD57 below 100 cells/μl of whole blood (mean±SE 49.12±3.12), and among them 47 (64.4%) patients showed CD57 below the lower limit of the normal range (the normal range is considered 60-360 cells/μl of whole blood).


Perforin mrna expression : A mean to evaluate nk cell activation
Since nk cells play a central role in the defense against bacteria and viruses, decreased nk activity can lead to the development of opportunistic infections.
Nk cells exert their cytotoxic effect by releasing perforin, a protein that will destroy the cytoplasmic membrane of target cells and finally kill them.
Increased perforin indicates that an infection is in place, while low perforin would indicate on ongoing persistent viral infection.
Inflammation
The response of our natural immunity to stress is called
Neutrophils and macrophages congregate at the site of injury/infection.
They phagocyte invaders and release toxic substances such as oxygen radicals.
Macrophages release pro-inflammatory cytokines IL-6 and TNFalpha to organize further inflammatory response.
Mast cells and eosinophils will be involved in parasitic defense and allergy.
Natural killer cells eliminante non-self cells by releasing toxic substances.


Immune response
Cellular immune response Th1
This is how we eliminate intracellular pathogens and non- self cells.
Humoral immune response Th2
This is our ability to produce antibodies to neutralize pathogens.
Th1 and Th2 should always be in balance!
Specific immunity
Th1 and Th2 produce and release cytokines that trigger a domino effect leading to an immune reaction:
Cytokines released by Th1 are: IL-2, IL-12, INFɣ, INFα and INFβ
Cytokines released by Th2 are: IL-4, IL-5, IL-10
Th1 cytokines suppress Th2 cytokines and vice versa
If the pathogen is defeated, the immune system returns to a balance between Th1 and Th2
Unfortunately, some conditions involve chronic activation or suppression of one of the two categories.

TH1/TH2 Balance
Th1/Th2 balance urine-based Th1/Th2 balance test
may detect disturbances of this delicate equilibrium in time in order to restore balance whenever required and before irreversible conditions are developing
allows patients to follow-up on Th1/Th2 balance during therapy (anti- oxydants, probiotics, nutraceuticals).

Cytokine imbalances in autism spectrum disorders
Ashwood et al. (Brain Behav Immun. 2011) reported on significant increases in plasma levels of a number of cytokines, including IL-1β, IL-6, IL-8 and IL-12p40 in the ASD group compared with controls.
Suzuki et al. (PLoS One 2011) reported that the plasma concentrations of IL-1β, IL-1RA, IL-5, IL-8, IL-12(p70), IL-13, IL-17 and GRO-α were significantly higher in subjects with ASD compared with the corresponding values of matched controls.
Okada et al. (Prog Neuropsychopharmacol Biol Psychiatry 2007) and Ashwood et al. (J Neuroimmunol. 2008 ) reported on decreased serum levels of transforming growth factorbeta1 (TGFb1) in patients with autism, with lower TGFb1 levels associated with lower adaptive behaviors and worse behavioral symptoms, suggesting that
Al-Ayadhi LY1, Mostafa GA – J Neuroinflammation. 2012 9:158. reported that Children with autism had significantly higher serum IL-17A levels than healthy controls (P <0.001), with increased serum levels of IL-17A found in 48.9% of the autism group.

Patients with severe autism had significantly higher serum IL-17A levels than those with mild to moderate autism (P=0.01), and raised serum IL-17A levels were significantly more common in children with severe autism (67.9%) than in those with mild to moderate autism (17.6%), P=0.001.
Serum IL-17A levels were raised in the group with autism, and the levels correlated significantly with the severity of autism
Further research is warranted to determine whether the increase of serum IL-17A levels plasma has a pathogenic role in autism, and whether anti- IL-17A therapy could be useful.
The importance of assessing inflammation-related markers

MIJATOVIC T. ET AL., 2018, AIMS MOLECULAR SCIENCE 5:173-182.
Pge2 production during illness and psychological stress

Quantification

PGE2 has been found as significantly higher in autistic patients
Quantification of serum levels of Prostaglandine E2
Prostaglandin E2 (PGE2) has been found as significantly higher in autistic patients, recording an increase of 91.15% (El-Ansary & Al- Ayadhi, Lipids Health Dis. 2012).
PGE2 is a compound derived from membrane phospholipids and is a key mediator of immunopathology in chronic infections and cancer
PGE2 selectively suppresses effector functions of macrophages and neutrophils and the Th1-, CTL-, and NK cell-mediated type 1 immunity, but it promotes Th2, Th17, and regulatory T cell responses.
PGE2 modulates chemokine production, inhibiting the attraction of proinflammatory cells while enhancing local accumulation of regulatory T cells cells and myeloid-derived suppressor cells.
Elastase mrna expression : a marker of inflammation

Elastase is an inflammatory protease expressed in immune cells (monocytes, neutrophils) that contributes to immune defense by inactivating foreign bacteria but at the same time it causes damage to connective tissue, breaks down cytokines, immunoglobulins and immune cells receptors. An excess, chronic production of elastase is therefore detrimental detrimental (destroyed gamma-globulins➔ decreased immunity; broken elastin➔diminished tissue elasticity, problems with neck) .
Environmental exposure and oxidative stress
Oxidative stress is implicated in a large number of diseases, including neurodegenerative diseases and autoimmune diseases
Indicators of oxidative stress have been detected in muscles and blood
Oxidative damage to cellular membranes can alter the permeability of the blood-brain barrier, which could lead to some of the cognitive symptoms observed in patients.
Increased oxidative stress could have several origins: chronic inflammation (activated neutrophils release pro-oxidative molecules), excess nitric oxide production (NO reacts with free radicals to produce peroxynitrite, a potent oxidant), or exposure to environmental toxins (exposure to certain chemicals leads to the depletion of essential antioxidants such as glutathione and selenium; heavy metals can also directly inhibit antioxidant enzymes like superoxide dismutase or glutathione reductase).
Oxidative stress markers are useful to evaluate the need for antioxidant therapy.

Summary – testing for immune and metabolic dysfunctions

The extent of the global immune and / or metabolic dysfunctions are evaluated by testing:
cytokine expression
elastase and perforin mRNA expression
oxidative stress, heavy metals, molds
macrophage phagocytic activity
alpha-N-acetylgalactosaminidase activity(Nagalase testing)
sCD14 expression
C3a & C4a expression
CD57 cell subset absolute count
prostaglandine E2 (PGE2) synthesis and hsCRP
VEGFsynthesis
ammoniaaccumulation
kynurenic and quinolinic acid accumulation, and many more
Testing for intestinal dysfunction in autism
Although ASD primarily impacts the brain, over recent years, links with other systems have become clear — in particular, gastrointestinal (GI) issues seem to occur more often in individuals with ASD than in the rest of the population.
The GI issues that come with ASD might be due to two factors: firstly, inappropriate immune activation, causing inflammation of the tract; and, secondly, differences in the types of gut bacteria that are present.

Gut-brain axis in autism


Intestinal dysfunctions in autism
Gut flora and gastrointestinal status in children with autism correlate with autism severity
Adams et al. (BMC Gastroenterology 2011) reported that gastrointestinal symptoms were strongly correlated with the severity of autism. From four types of beneficial bacteria that were investigated, the children with autism had much lower levels of Bifidobacterium (-45%), slightly lower levels of Enterococcus (-16%), and much higher levels of Lactobacillus (+100%).
Finegold et al. (Anaerobe 2010) reported that in the control children’s stools, Firmicutes accounted for 63.6% of the total flora but only 38-39% of the flora of autistic children’s stools. Bacteroidetes accounted for 30% of the stool flora in controls and for 51% in the flora of stools of autistic children. Actinobacteria made up 1.8% of stool flora of control children and between 0.4 and 0.7% of the flora of autistic children. Proteobacteria made up 0.5% of the flora of control children and between 2.3 and 3.1% of the flora of autistic children. In summary, the fecal flora of autistic children was statistically significantly different from the fecal flora of healthy children.
R.E.D. Laboratories are offering specialty test to deeply analyze gut microbiota: msa assay
Metagenomic stool assay (MSA)
Intestinal microbiota analysis : from culture to high-throughput sequencing:
Until recently research into microbiota composition relied almost exclusively on culture ; 40 to 80% of gut bacteria cannot be cultured
Identification of colonies can be difficult
Bacteria must be alive: studies of anaerobes very difficult, major loss during collection and processingof samples
Culture approach may address only a small fraction of all bacterial species (10%?)
E.coli once thought to be a dominant species, is a minor member…
R.E.D. Labs scientists have developed and validated a new procedure to analyze bacterial populations in a stool sample : MSA assay
New molecular technique involving sequencing of specific regions of bacterial DNA (metagenomics)
Can be performed on dead organisms (exposure to oxygen, freezing are not a problem)
Identification of each bacteria by comparing sequence with public databases: extremely precise, not subjective
High-throughput technology allows identification of tens or even hundreds of thousends organisms in a single sample
Bacterial DNA was extracted from stool samples, PCR amplification was performed on 16S rRNA gene regions, and PCR amplicons were sequenced Bacteria were classified by phylum, family and genus.


ASD Child MSA
Prevotella: strong hydrogen sulfide (H2S) producers. In excess, H2S acts as a mitochondrial poison and a potent neurotoxin. It can directly inhibit enzymes involved in the cellular production of energy. H2S also interferes with oxygen transport by blocking hemoglobin in the red blood cells. Finally, H2S is lowering gut pH preventing the growth of many beneficial bacteria,/p>
Bacteroides: dysbiotic bacterias found in most anaerobic infections with an associated mortality of more than 19 %. Species of the genus Bacteroides have the most antibiotic resistance mechanisms and the highest resistance rates of all anaerobic pathogens.


1st visit April 2017: High both Bacteroides & Prevotella
2nd visit December 2017:Still high Bacteroides but normalized Prevotella
3rd visit December 2018:Normalized both Bacteroides and Prevotella
Leaky gut in asd children

Leaky gut
ZONULIN ELISA test in stool samples
Zonulin is the “doorway” to leaky gut. Zonulin opens up the spaces between the cells of the intestinal lining. When leaky gut is present, the spaces between the cells open up too much allowing larger protein molecules and bacteria to get into the bloodstream where an immunologic reaction can take place. As the zonulin level rises, the seal between the intestinal cells diminishes. Zonulin is the only physiological modulator of intercellular tight junctions described so far that is involved in trafficking of macromolecules and, therefore, in tolerance/immune response balance.


Consequences of the leaky gut – chronic activation (inflammation) of immune system
Lipopolysaccharide (LPS) – bacterial compound that can easily make its way to the blood.
Present in the bloodstream LPS will induce a strong pro-inflammatory response in monocytes and macrophages, involving recognition by a receptor (Toll-like receptor-4) and the subsequent secretion of cytokines such as IL-1, IL-6, TNF-alpha.
LPS also induces the NK-kB-mediated production of nitric oxide. Because NO is increased, NK function is inhibited and opportunistic infections such as mycoplasma infections are often observed.
Herpesviruses, which tend to reactivate in a context of immune activation, will also be frequently detected.
Consequences of the leaky gut

SCD14 – An interesting marker

Patients with severe autism had significantly higher serum IL-17A levels than those with mild to moderate autism (P=0.01), and raised serum IL-17A levels were significantly more common in children with severe autism (67.9%) than in those with mild to moderate autism (17.6%), P=0.001.
Serum IL-17A levels were raised in the group with autism, and the levels correlated significantly with the severity of autism
Further research is warranted to determine whether the increase of serum IL-17A levels plasma has a pathogenic role in autism, and whether anti- IL-17A therapy could be useful.
Toxic metabolites from bacteria
D-lactate in serum
a product of bacterial metabolism, it is neither produced nor metabolized by mammalian cells. Typically, elevated D-lactate levels are due to bacterial infection or short bowel syndrome in humans. Due to slow metabolism and excretion, high D-lactate can cause acidosis and encephalopathy.


Ammonia in serum
Ammonia is derived from bacterial enzymatic action on ingested amino acids. It is absorbed from the gastrointestinal tract and delivered through the portal vein to the liver, which converts most of it into urea. Abnormally high levels of ammonia can result from colic or “enteric hyperammonemia” (combination of increased bacterial production and increased gut permeability) that occurs despite normal hepatic function. Hyperammonemia is a metabolic condition characterized by elevated levels of ammonia in the blood. Increased entry of ammonia to the brain is a primary cause of neurologic disorders, metabolic disorders and some toxic encephalopathies.
Intestinal inflammation in autism
Autismandgastrointestinal
Several reports have revealed a high prevalence of gastrointestinal symptoms, (reviewed by Horvath and Perman, Curr Gastroenterol Rep. 2002).
Mild to moderate degrees of inflammation were found in both the upper and lower intestinal tract. In children with ASD, the presence of GI dysfunction is often associated with increased irritability, tantrums, aggressive behavior, and sleep disturbances (reviewed by Critchfield et al., Gastroenterol Res Pract. 2011).

Stool-based assays for intestinal inflammation

sIgA ELISA test in stool sample
sIgA key function is to bind to invading micro organisms and toxins and entrap them in the mucus layer or within the epithelial cells, so inhibiting microbial motility, agglutinating the organisms and neutralizing their exotoxins and then assist in their harmless elimination from the body in the fecal flow.
The concentration of sIgA gives us information about the intestinal immune defense:
A lack of sIgA indicates a diminished activity of the intestinal immune system.
An increase level of sIgA shows intestinal inflammation.
beta-Defensin-2 ELISA test in stool samples
Defensins exert a variable degree of antimicrobial activity against bacteria, fungi, and some enveloped viruses. The expression of ß-defensins is induced by the pro-inflammatory cytokines and also through microorganisms (e.g. E. coli, H. pylori or P. aeruginosa) and by probiotic microorganisms. A ß-defensin-2 deficiency can, for example, be observed in the intestinal mucous of patients with Crohn’s disease. The defense system of the mucous membrane is therefore restricted and allows an increased invasion of bacteria, which could possibly lead to a typical infection in Crohn’s disease patients.
Recent results imply that ß-defensin-2 is overexpressed in active intestinal inflammation especially in ulcerative colitis.
EDN / EPX ELISA test in stool samples
The accumulation of EDN in the intestine is associated with inflammation and the tissue damage. Fecal EDN is considered the best of the cytotoxic granule proteins for assessment of gut inflammation. Elevated levels of fecal EDN are linked to multiple inflammatory conditions, like food allergy/sensitivity, pathogenic infections (C. difficile and H. Pylori), IBS, Eosinophilic Gastrointestinal Disorders.
Inflammation markers in stool samples
Hemoglobin : discharged with the feces in gastrointestinal bleeding diseases
Transferrin: a blood-derived component ; a good marker for gastrointestinal bleeding
Calprotectin: a neutrophil cytosolic protein with antimicrobial properties, which is present at increased concentration in stool during bowel inflammation.
Lactoferrin: a primary component of the acute inflammatory response released from fecal leukocytes; may serve as marker of inflammation in the intestine.

The importance of assessing intestinal dysfunctions

MIJATOVIC T. ET AL., 2018, AIMS MOLECULAR SCIENCE 5:173-182.
Assays for intestinal infections

INFECTIONS – assessment in stool samples
Ag-based testing for Clostridium, Yersinia, Enterovirus, Parasites, etc
INFECTIONS – PCR-based viral and bacterial assessment in intestinal biopsies
Importance of testing for gastrointestinal disorders
GI symptoms may overlap with ASD core symptoms through different mechanisms.
Shared pathogenetic factors and pathophysiological mechanisms possibly linkingASD and GI disturbances, as shown by most recent studies, include among others
Intestinal inflammation with or without autoimmunity,
Intestinal permeability,
Food allergies,
Dysbiosis
Dysregulation of the gut microbiome has also been shown to be involved in modulating GI functions with the ability to affect intestinal permeability, mucosal immune function, and intestinal motility and sensitivity.
Immune dysregulation, GI inflammation, dysbiotic microbiome and dietary metabolites may contribute to brain dysfunction and neuroinflammation. Unexplained worsening of nonverbal behaviors (agitation, anxiety, aggression, self-injury, sleep deprivation) should alert professionals about this possibility.

Summary – testing for gastrointestinal disorders

Useful assays to investigate intestinal dysfunctions:
BLOOD-BASED Tests: sCD14, Ammonia concentration, Lactase deficiency assay, D-lactate
BIOPSY-BASED Tests: PCR-based detection of viral and bacterial infections
STOOL-BASED Tests:
Intestinal Inflammation markers in stool samples: sIgA, Beta-2 Defensin, EPX / EDN, inflammation markers in stool samples
! Gut inflammation contributes to increased bacterial translocation.
Intestinal Infections : immunochromatography antigenic testing for intestinal infection
Leaky gut: ZONULIN ELISA test in stool samples
Dysbiosis: MSA assay (metagenomic stool test)
High Prevotella : gut acidification; H2S production ➔ mitochondrial collapse,
Low Bifidobacterium: Bifido cannot stand low pH
High Clostridium IV ➔ production of toxic metabolites
Enterococcus – facultative anaerobes, if inflammation ➔ overgrowth
Testing for infections /chronic infections

Tick-borne infections and autism
An association between Lyme disease (LYD) and other tick-borne infections (TBI) during fetal development and in infancy with autism, autism spectrum disorders (ASD) and autistic symptoms has been noted by numerous clinicians and parents.
Treatment of TBI during pregnancy can prevent the development of ASD associated with TBI (Bransfield et al., Med. Hypotheses 2008),
Bransfield et al. wrote in 2008 a review paper (Med. Hypotheses 2008) to collate information from conference presentations on this issue with other sources that further address this association. They indicated that the preliminary data suggests Borreliosis may be a contributor in 20– 30% of ASD, and pathogenic Mycoplasma may be a contributor in 58%.
Autism spectrum disorder results from multiple etiologies with both genetic and environmental contributions, including at least 23 different infections, seven of which are chronic infections (Babesia, Bartonella, B. burgdorferi, Ehrlichia, Human Herpesvirus-6, Chlamydia pneumoniae and Mycoplasma), and the immune reactions associated with these infections (Bransfield, Pediatr Health 2009).


Lyme disease testing
Importance to enlarge borreliosis-related testing targets (i.e. not testing only for B. burgdorferi sl)
The overall high expansion of undiagnosed Lyme disease cases worldwide might be linked to the screening choice focusing only on B. Burgdorferi sl and only rarely testing for B. miyamotoi while the later one seems to be much more prevalent. Searching for actual bacterial presence using phage – based testing might pacify the debate and controversies on testing choices and late/chronic stage patients.
Importance of novel testing approaches
The overall high failure rate of tick-borne infection (TBI)-related testing underscores the necessity for novel approaches, i.e. not relying on serology and two-tier testing.
Novel testing approaches – phage-based test
The importance of novel testing approaches
Phelix Phage Borrelia detection method (Patent WO2018083491A1) consists of targeting the presence of outnumbered prophages part of the bacteria lysogenic cycle. Bacteriophages are present only on active bacterial infections; hence a phage- based test is a direct proof of an active infection.
The lysogenic cycle: The phage infects a bacterium and inserts its DNA into the bacterial chromosome, allowing the phage DNA (now called a prophage) to be copied and passed on along with the cell’s own DNA.
The lytic cycle: The phage infects a bacterium, hijacks the bacterium to make lots of phages, and then kills the cell by making it explode (lyse).


Phelix phage borrelia test
Bacteriophages could become a novel testing approach tool based on the principle that if there are phages it is because there are living bacteria.
Phelix Charity together with Leicester University microbiology department have recently developed a Borrelia Phage-based PCR test searching for 3 major
Borrelia groups:
Borrelia burgdorferi sl (including B. burgdorferi ss, B. afzelii, B. garinii, B. spielmanii, etc)
Borrelia miyamotoi and
Relapsing fever group (B. recurrentis, B. hermsii, etc).
This method is efficiently used to assess both human samples and ticks.
Highly sensitive and specific.
Do not generate positive signal against other bacterial strains.
False positive are ruled out by sequencing.

Immune dysfunction in TBD
A hallmark of chronic Lyme disease is an underlying immune dysfunction that not only limits the ability to accurately diagnose Lyme, leaving many such patients misdiagnosed, but also serves as a major reason for lack of treatment response to antibiotics with an inability to eradicate the chronic infection.
The Borrelia bacteria (cause of Lyme disease) transforms from an acute to a chronic infection by transforming the body to a TH2 “extracellular” dominant response and then converting from a free swimming spirochete form in the blood into an intracellular form (L-form) to escape the elevated TH2 immunity. The suppressed and down-regulated TH1 intracellular immune response becomes an ineffective immune response by the body and an effective evasion strategy, which is the hallmark of transformation to late-stage Lyme dissemination.
Appropriate immune modulating therapies that are able to restore normal functioning immunity may be the biggest necessary leap forward in the development of an effective treatment protocol for this multi-system illness.

Mycoplasma ssp., human hv6 coinfections, intracellular pathogens in asd
Nicolson et al. (J Neurosci Res. 2007) examined the blood of 48 patients from central and southern California diagnosed with autistic spectrum disorders (ASD) and found that a large subset of ASD patients shows evidence of bacterial and/or viral infections.
a large subset (28/48 or 58.3%) of patients showed evidence of Mycoplasma spp. infections compared with two of 45 (4.7%) age-matched control subjects.
the prevalence human herpes virus-6 (HHV-6, 14/48 or 29.2%) coinfections in ASD patients versus 4/48 or 8.3% in Control subjects.
As reported by Blinstock (Med. Hypotheses 2001), several autism- spectrum subgroups derive from intra-monocyte pathogens such as measles virus, cytomegalovirus, human herpesvirus 6, and Yersinia enterocolitica. In some such children, one or more of these pathogens persists as a chronic-active, seemingly subclinical infection etiologically significant to the child’s autistic traits. Within these subgroups, immune impairments and atypical infections may be treatable.
A vicious circle

Conclusions
More and more evidence points towards a combination of factors (genetic, infectious, environmental, etc.) being important in the development of chronic immune dysfunctions, the cardinal finding in autistic patients.
In many countries ASD are still considered as psychiatric despite clear biomedical evidence.
For better management of this affliction suffering from lack of medical recognition, need to consider SPECIALTY TESTS
Based on the recent publications and extensive collaborations with MDs specialized in management of autism-related disorders, we developed dedicated testing offer focusing on:
global immune dysfunctions
persistent and/or chronic infections, especially tick-borne infection
intestinal dysfunctions and intestinal inflammation
Wider network of new collaborations needed for further advancement in autism biomarkers deciphering and validation

Integrative approach for testing patients with late / persistent / chronic tick-borne infections (TBI)
Vector-borne infections are increasing globally.
The most known, and most investigating concern borreliosis, bartonelosis, babesiosis, rickettsiosis and anaplasmosis. Many other pathogens can worsen the clinical picture and further complicate differential diagnosis.
Read our updated summary, available in different languages ( www.redlabs.com)
Tick-borne infections
Tick-borne diseases, which afflict humans and other animals, are caused by infectious agents transmitted by tick bites.➔Whenever possible, get the tick tested by PCR
Tick-borne illnesses are caused by infection with a variety of pathogens.
Tick-borne infections are increasing globally – Lyme disease is among the most prevalent vector borne infection in the U.S. and Europe and is reaching epidemic levels (Kugeler et al. 2015; Sykes et al. 2014).
Download our TICK AWARENESS BROCHURE available in different languages
(see www.redlabs.com)

Tick awareness brochure (1)

Tick awareness brochure (2)

Tick awareness brochure (3)

Tick awareness brochure (4)


Tick-borne infections
Lyme disease is the most widely known tick-borne disease and is caused by bacteria of the genus Borrelia.
Because individual ticks can harbor more than one disease-causing agent, patients can be infected with more than one pathogen at the same time, compounding the difficulty in diagnosis and treatment.
Among neglected infections, there are few that deserve more attention and investigations, like Tularemia, Yersinia, Mycoplasma, Chlamydia, Epstein-Barr virus and Herpesviruses. Our data show that prevalence of these infections are not negligible and they should be more investigated.
Remember
It is important to bear in mind that TBD can be acute or late stage / persistent / chronic; this is important given the novel testing and treatment approaches might be different in these two situations.
Lyme disease exhibits a variety of symptoms that may be confused with immune and inflammatory disorders.
If an individual has any chronic health condition, ranging from arthritis to chronic fatigue syndrome to fibromyalgia, it is important to rule out or diagnose tick-borne disease(s). It is apparent that many cases of fibromyalgia and chronic fatigue syndrome are actually TBD in disguise
Chronic patients have complex clinical picture with multiple afflictions needing thus multiple testing and careful interpretation of testing results.
Chronic lyme diseas
Chronic Lyme disease can mimic every disease process including Chronic Fatigue Syndrome (Myalgic Encephalomyelitis), Fibromyalgia, Autoimmune conditions including sero-negative rheumatoid arthritis and MS, Psychiatric conditions including depression and anxiety, and cause significant memory and concentration problems mimicking early dementia. It is called the “Great Imitator“
If an individual has any chronic health condition, ranging from arthritis to chronic fatigue syndrome to fibromyalgia, it is important to rule out or diagnose Lyme disease. It is apparent that many cases of fibromyalgia and chronic fatigue syndrome are actually Lyme disease in disguise
Chronic Lyme sufferers also frequently house “co-infections” such as Mycoplasma, Chlamydias, Ehrlichia, Bartonella and Babesia. These are different types of “bugs” that enjoy the company of B. burgdorferi

Remember
The overall high failure rate of therapies for vector-borne infections, especially in late/persistent/chronic patients, underscores the necessity to fully investigate different concurrent infections along with resulting gastrointestinal and immune dysregulations.
It is important to investigate different “co-infections” (i.e. tick- borne infections) but also other opportunistic infections (viral, bacterial, parasitic).

Testing for tick-borne infections
Diagnosing Lyme and TBI-related diseases is extremely challenging.
TBI diagnosis complications are a result of inadequate testing, mainly focusing on markers for the disease’s early stages.
Lyme cases are commonly misdiagnosed with other illnesses and even when a proper diagnosis is made, it’s often difficult to verify because accurate testing isn’t always available.
Very few tests for Tick-borne diseases (TBD) are approved for clinical diagnosis, thus most of available testing options are “investigational” or “research” tests, aiming to help the assessment of patients with Lyme-like complaints.
Integrative approach for tbd testing: part 1 – pathogen detection


Currently used tests for borrelia detection and their limitations

Need for new tests development

Cooperation between academia, testing lab and medical specialists



Novel testing approaches : phage-based test
The importance of novel testing approaches
The overall high failure rate of tick-borne infection (TBI)-related testing underscores the necessity for novel approaches, i.e. not relying on serology and two-tier testing. Phelix Phage Borrelia detection method (Patent WO2018083491A1) consists of targeting the presence of outnumbered prophages part of the bacteria lysogenic cycle.
Bacteriophages are present only on active bacterial infections; hence a phage-based test is a direct proof of an active infection.
The lysogenic cycle: The phage infects a bacterium and inserts its DNA into the bacterial chromosome, allowing the phage DNA (now called a prophage) to be copied and passed on along with the cell’s own DNA.
The lytic cycle: The phage infects a bacterium, hijacks the bacterium to make lots of phages, and then kills the cell by making it explode (lyse).


Phelix phage borrelia test
Bacteriophages could become a novel testing approach tool based on the principle that if there are phages it is because there are living bacteria.
Phelix Charity together with Leicester University microbiology department have recently developed a Borrelia Phage-based PCR test searching for 3 major Borrelia groups:
Borrelia burgdorferi sl (including B. burgdorferi ss, B. afzelii, B. garinii, B. spielmanii, etc)
Borrelia miyamotoi and
Relapsing fever group (B. recurrentis, B. hermsii, etc).
This method is efficiently used to assess both human samples and ticks. Highly sensitive and specific.
Do not generate positive signal against other bacterial strains.
False positive are ruled out by sequencing.

Reminder on available testing approach methods

Chronic lyme disease and co-infections
Chronic lyme disease and co-infections
In Lyme disease concurrent infections frequently occur. Co-infecting agents can be transmitted together with Borrelia burgdorferi by tick bite resulting in multiple infections but a fraction of co-infections occur independently of tick bite.
Clinically relevant co-infections are caused by Bartonella species, Yersinia enterocolitica, Chlamydophila pneumoniae, Chlamydia trachomatis and Mycoplasma pneumoniae.
Infections caused by these pathogens in patients not infected by Borrelia burgdorferi can result in clinical symptoms similar to those occurring in Lyme disease. This applies particularly to infections caused by Bartonella henselae, Yersinia enterocolitica, and Mycoplasma pneumoniae. Chlamydia trachomatis primarily causes polyarthritis. Chlamydophila pneumoniae not only causes arthritis but also affects the nervous system and the heart, which renders the differential diagnosis difficult. The diagnosis is even more complex when co-infections occur in association with Lyme disease. (from Berghoff W. Open Neurol J. 2012;6:158-78.)
Lyme disease exhibits a variety of symptoms that may be confused with immune and inflammatory disorders.

Integrative approach for tbd testing: part 1 – pathogen detection

Phelix phage borrelia test
Immunoblot for Borrelias, Chlamydias (pneumoniae, trachomatis, psittacii), Yersinia, EBV, Parvovirus, Treponema, Tropical fever (Chikungunya virus + Dengue fever virus + Zika virus), Hepatitis E Virus, etc
Serology tests for CMV, Toxoplasmosis, Tularemia, Leptospira, BrucellaCapt
FISH test for Babesia
PCRs for Mycoplasma spp, Mycoplasma fermentans, Mycoplasma pneumoniae, Bartonella, Brucella, Coxiella, Babesia, Anaplasma, Ehrlichia, Chlamydias, Rickettsias, Midichloria mitochondrii, etc
PCRs for viral infections: herpesviruses like HHV-6, HHV-7, HHV-8, Parvovirus, EBV, Cytomegalovirus, Tick-borne encephalitis virus, West Nile virus, Coxsacki virus, Enterovirus
MOLDS Serology: IgG against 6 major molds: Candida albicans, Cladosporium herbarum, Aspergillus niger, Alternaria alternate, Penicillium chrysogenum, Aspergillus fumigatus
Quantification of mycotoxins in urine
Testing for parasites
New tests in development

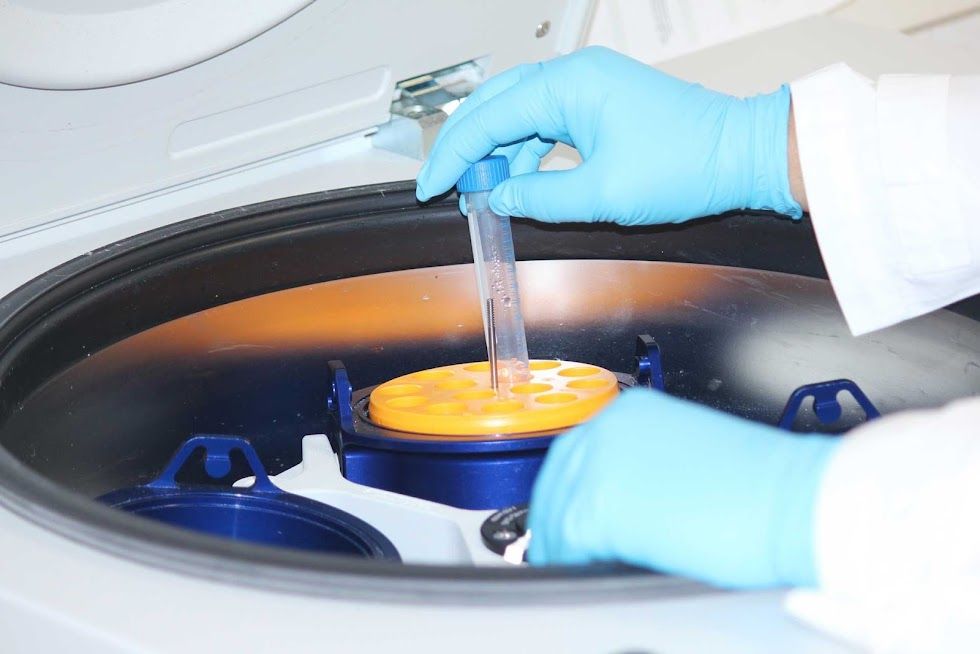
Yersinia
The bacteria from the genus Yersinia are Gram-negative enterobacteria. From the 17 described species there are 3 know to be human pathogens:
Yersinia pestis causes bubonic and pneumonic plague. Bubonic plague is transmitted by the bite of infected rat fleas. Swollen, blackened lymph nodes (buboes) develop, followed by septicemia and hemorrhagic pneumonia and death. The pneumonic form spreads directly from human to human via respiratory droplets. Outbreaks are explosive in nature, and invariably lethal.
Yersinia enterocolitica causes severe diarrhea and local abscesses
Yersinia pseudotuberculosis causes severe enterocolitis.
The most common source of Y. enterocolitica infection in humans is pork (raw or undercooked) and also contaminated water, meat, or milk.
Other strains of Yersinia are also found in many other animals including rodents, rabbits, sheep, cattle, horses, dogs and cats.
Yersinia pseudotuberculosis is a Gram-negative bacterium that causes Far East scarlet-like fever in humans.
Y. pseudotuberculosis infections can mimic appendicitis, the disease may cause skin complaints (erythema nodosum), joint stiffness and pain (reactive arthritis), or spread of bacteria to the blood (bacteremia). Y pseudotuberculosis causes severe intestinal abscesses
Genetically, the pathogen causing plague, Y. pestis, is very similar to Y. pseudotuberculosis. The plague appears to have evolved from Y. pseudotuberculosis
Common symptoms are:
Fever
abdominal pain, and
diarrhea (which is often bloody)
Complications include:
Joint pain
rashes (erythema nodosum)
Some persons present mild symptoms thus difficult to uncover.
Yersinia infections are sometimes followed by chronic inflammatory diseasessuch as arthritis, erythema nodosum, and reactive arthritis.
Yersinia may be associated with Crohn’s disease
Yersinia pseudotuberculosis-derived mitogens (YpM) are superantigens, which are able to excessively activate T cells by binding to the T cell receptor. Since YpM can activate large numbers of the T cell population, this leads the release of inflammatory cytokines.
The importance of testing for yersinia

“These repeated and unregulated inflammatory challenges may profoundly remodel the immune system and thereby contribute to the increased burden of autoimmune and inflammatory disorders.
Together, this study provides a framework to understand how previously encountered infections can induce a breakdown of tissue immune homeostasis, thereby contributing to disease later in life. Thus, in order to fully comprehend the etiology of complex diseases, it may be necessary to look beyond a patient’s genetic susceptibilities and concurrent environmental stressors and examine whether immunological scarring associated with previous infections may have ‘set the stage’ for chronic inflammation.“
These repeated and unregulated inflammatory challenges may profoundly remodel the immune system and thereby contribute to the increased burden of autoimmune and inflammatory disorders.”

Yersinia – testing results
Yersinia immunoblot tests make it possible to detect past Yersinia infections, and are thus ideally suited for identification of Yersinia-induced immunopathological complications and chronic yersiniosis. Detection of IgG and IgA antibodies can be a very useful testing tool if Yersinia-induced arthritis is suspected.
An immunoblot for the detection of IgG and IgA antibodies against all pathogenic Yersinia by means of Yersinia outer proteins (YOPs). Serological differentiation of Y. enterocolitica and Y. pseudotuberculosis infections is possible for the first time with the use of new species-specific Yersinia antigens (PsaA, MyfA).
Testing period : May 1st 2015 – May 1st 2019 (4 years)
Immunoblot on serum
Total tested: 2396 samples
IgA positive: 412 (➔17.2%)
IgG positive: 946 (➔39.5%)Total tested: 2396 samples
IgG, no differentiation: 624 positives (➔66% of IgG positives; 26.1% of all tested
IgG Y. pseudotuberculosis: 202 positives (➔21.4% of IgG positives; 28.4% of all tested
IgG Y. enterocolitica: 120 positives (➔12.6% of IgG positives; 5% of a2l8l tested
Tularemia
Tularemia, also known as rabbit fever, is an infectious disease caused by the bacterium Francisella tularensis
People can become infected in several ways, including:
Tick and deer fly bites
Skin contact with infected animals
Drinking contaminated water
Inhaling contaminated aerosols or agricultural and landscaping dust: can occur during farming or landscaping activities, especially when machinery (e.g. tractors or mowers) runs over infected animals or carcasses
Laboratory exposure
People could be exposed as a result of bioterrorism.

Tularemia is not known to be spread from person to person. People who have tularemia do not need to be isolated.
The diagnosis of tularemia is often delayed. It may take a significant length of time to diagnose and the condition and the disease may become complicated.
Some persons present mild symptoms thus difficult to uncover.
Symptoms vary depending how the person was infected:
Ulceroglandular: occurs following a tick or deer fly bite or after handing of an infected animal. A skin ulcer appears at the site where the bacteria entered the body. The ulcer is accompanied by swelling of regional lymph glands
Glandular: Similar to ulceroglandular tularemia but without an ulcer. Also generally acquired through the bite of an infected tick or deer fly or from handling sick or dead animals.
Oculoglandular: occurs when the bacteria enter through the eye. This can occur when a person is butchering an infected animal and touches his or her eyes. Symptoms include irritation and inflammation of the eye and swelling of lymph glands in front of the ear.
Oropharyngeal: results from eating or drinking contaminated food or water. Patients with orophyangeal tularemia may have sore throat, mouth ulcers, tonsillitis, and swelling of lymph glands in the neck.
Pneumonic: the most serious form of tularemia. Symptoms include cough, chest pain, and difficulty breathing. This form results from breathing dusts or aerosols containing the organism. It can also occur when other forms of tularemia (e.g. ulceroglandular) are left untreated and the bacteria spread through the bloodstream to the lungs.
Typhoidal : characterized by any combination of the general symptoms (without the localizing symptoms of other syndromes)

Tularemia – testing results
Testing period : July 1st 2015 – May 1st 2019
Screening test : immunochromatography on serum
Total tested: 1769 samples
392 (= 22.16%) were found positive and undergo confirmatory testingTotal tested: 1769 samples
Confirmatory test: IVD Tularemia IgM ELISA
392 went to confirmatory testing
87 were found borderline (22,2% among those that went for confirmatory testing, 5 % of total tested samples)
117 were found positive (29,8% among those that went for confirmatory testing, 6,6% of total tested samples)
Herpes viruses – HHV6 & HHV7
HHV-6 has a very high prevalence (close to 100% of the world’s population has been exposed); primary infection is often associated with a febrile condition and sometimes with the onset of roseola (exanthem subitum).
HHV-6 has immunomodulatory effects, including suppression of T-cell proliferation and alteration of cytokine production.
This immunosuppression may favor the development or progression of other viral infections such as CMV, EBV or HIV.
HHV6 qPCR test : 3% of tested blood samples (509 samples) were found positives with high viral load, and 13% of them present HVV6 chromosomal integration.

HHV-7 is closely related to HHV-6, primary infection usually occurs later in childhood than HHV-6 infection; it can also cause exanthem subitum.
HHV-7 efficiently infects and replicates in CD4+ cells; it can be found in brain tissue but at a lower frequency than HHV-6.
It has been suggested that HHV-7 could reactivate HHV-6 from latency. Increased prevalence has been reported in people with autoimmune disease.Some persons present mild symptoms thus difficult to uncover.
HHV7 qPCR test : 34,4% of tested blood samples (128 samples) were found positives with high viral load.
Given that a majority of the population has been exposed to HHV, qPCR testing is to be preferred over serology testing.

Ebv-epstein-barr virus
EBV (HHV-4) infects more than 90% of the world’s adult population.
It is transmitted by salivary contact; the virus first replicates in the epithelium of the oropharynx before infecting B lymphocytes where it will persist for life in a latent state.
EBV re-activation is known to occur in times of immunocompromised state, cellular stress, and inflammation.
Following initial infection, EBV can reactivate and has been shown to have many connections with various chronic illnesses.
Epstein-Barr virus infection is known to cause false-positive results in Lyme disease serologic testing, particularly IgM tests.
EBV immunoblot test (393 samples tested):
IgM positive samples: 3%
IgG positive samples: 85%, 2% with recent infection
IgG positive: 946 (➔39.5%)Total tested: 2396 samples
qPCR testing should be added to serology testing.
Mycoplasma
Ticks were found to carry M. Pneumonae, M. Genitalium & M. Fermentans
These infections are exacerbating the CTBI patients, especially those with auto-immune manifestations.
Mycoplasma spp cause B cells to be overstimulated, promoting auto-immune and rheumatoid Disease
Mycoplasma increase production of IL-1beta & IL-6
Poor treatment results with antibiotics
PCR testing in body fluids and biopsies preferred to serology testing
PCR testing of sputum and swaps (total 111 samples) with confirmatory sequencing: 28.8% positives


Chlamydia
Ticks DO NOT carry Chlamydia BUT reactivate in presence of T.B.I.
C. Pneumonae
C. Trachomatis
C. Psittaci
HP60 is expressed ➔ arthritis, drive auto-immune reactions, create free radicals and oxidative stress
Chlamydia ➔ turns on NF kappa B ➔cytokine/inflammatory molecules
An immunoblot for the detection of IgG and IgA antibodies against Chlamydia trachomatis, Chlamydophila pneumoniae and Chlamydophila psittacci:
1927 tested samples:
IgA Chlamydophila pneumoniae: 9.8% positives
IgA Chlamydophila psittacci: 0.4 % positives
IgA Chlamydila ptrachomatis: 6.7% positives
Integrative approach for tbi part 2 – intestinal dysfunctions

Intestinal dysfunctions
Regulation of immune function in the gut
80% of our immune cells reside in the gut
Gut associated lymphoid tissue (GALT) is spread along the intestinal mucosa (Peyer’s patch in the small intestine, lymphoid follicles in the colon) and hosts 80% of the body’s immune cells
These immune cells permanently interact with mucosa-associated micro- organisms (bacteria, viruses…)
A delicate balance is maintained between tolerance to gut antigens (down- regulation of inflammation,…), and defense against pathogens (production of defensins,…)
Imbalance of gut immunity affects the whole body
Gut barrier integrity is essential : Increased permeability of the mucosa causes systemic endotoxemia (chronic low grade inflammation) and abnormal immune reactions to gut antigens
Interactions host/gut flora : the gut microbial flora plays a major role in maintenance of host health, but can be affected by abnormal host immune function

Tbi and gastrointestinal disorders
Signs and symptoms related to the gastrointestinal tract and liver may provide important clues for the diagnosis of various tickborne diseases

FROM: GASTROINTESTINAL AND HEPATIC MANIFESTATIONS OF TICKBORNE DISEASES IN THE UNITED STATES SYED ALI ZAIDI & CAROL SINGER, CLIN INFECT DIS. 2002;34(9):1206-1212. DOI:10.1086/339871

Lyme disease and gastrointestinal disorders
Patients with Lyme and TBDs may present primarily with GI manifestations.
2015 ILADS conference, Dr. Farshid Rahbar: These patients may have complex or persistent GI symptoms involving upper, mid, or lower GI tract and have already been treated for GI issues
Bloating/Gas: in 76% of patients Abdominal Pain: in 48% of patients
Constipation: in 42% of patients
Food Intolerance: in 42% of patients
Irregular Bowel Movements: in 37% of patients
The number of patients presenting with such symptoms is probably reaching epidemic proportions.
Testing for gastrointestinal problems need to be included
Useful assays to investigate intestinal dysfunctions:
BLOOD-BASED Tests: sCD14, Lactase deficiency assay, D-lactate, Ammonia in serum
BIOPSY-BASED Tests: PCR-based detection of viral and bacterial infections
STOOL-BASED Tests:
Intestinal Inflammation: sIgA, Beta-2 Defensin, EPX / EDN, Inflammation markers in stool samples
Intestinal Infections : immunochromatography antigenic testing for intestinal infections
Leaky gut: ZONULIN ELISA test in stool samples
Dysbiosis: MSA assay (metagenomic stool test)

Blood-based assays for intestinal dysfunctions

sCD14 in serum
sCD14 is expressed in monocytes/macrophages and plays a critical role in the recognition of bacterial cell wall components (LPS). The extracellular part of CD14 can be cleaved and released in the plasma, where it will inactivate circulating LPS. Serum soluble CD14 levels are significantly elevated in patients with leaky gut, inflammatory bowel disease, Crohn’s disease, but also in patients suffering from Brucellosis or Lyme disease.
Lactase deficiency assay
a polymorphism in the gene coding for lactase, an enzyme responsible for the digestion of lactose (C/T- 13910 polymorphism). In affected people, production of the enzyme declines during or shortly after childhood, resulting in lactose malabsorption. Undigested lactose sugars affect the development of gut microflora, leading to dysbiosis.
D-lactate in serum
a product of bacterial metabolism, it is neither produced nor metabolized by mammalian cells. Typically, elevated D-lactate levels are due to bacterial infection or short bowel syndrome in humans. Due to slow metabolism and excretion, high D-lactate can cause acidosis and encephalopathy.
Ammonia in serum
Ammonia is derived from bacterial enzymatic action on ingested amino acids. It is absorbed from the gastrointestinal tract and delivered through the portal vein to the liver, which converts most of it into urea. Abnormally high levels of ammonia can result from colic or “enteric hyperammonemia” (combination of increased bacterial production and increased gut permeability) that occurs despite normal hepatic function. Hyperammonemia is a metabolic condition characterized by elevated levels of ammonia in the blood. Increased entry of ammonia to the brain is a primary cause of neurologic disorders, metabolic disorders and some toxic encephalopathies.


Consequences of the leaky gut – chronic activation (inflammation) of the immune system
Leaky gut testing (Zonulin in stool) : 3 years testing period, 1301 samples 63.87% patients with increased levels!!
Lipopolysaccharide (LPS) – bacterial compound that can easily make its way to the blood.
Present in the bloodstream LPS will induce a strong pro-inflammatory response in monocytes and macrophages, involving recognition by a receptor (Toll-like receptor-4) and the subsequent secretion of cytokines such as IL-1, IL-6, TNF-alpha.
LPS also induces the NK-kB-mediated production of nitric oxide. Because NO is increased, NK function is inhibited and opportunistic infections such as mycoplasma infections are often observed.
Herpesviruses, which tend to reactivate in a context of immune activation, will also be frequently detected.
Consequences of the leaky gut

Stool-based assays for intestinal inflammation

sIgA ELISA test in stool samples
sIgA key function is to bind to invading micro organisms and toxins and entrap them in the mucus layer or within the epithelial cells, so inhibiting microbial motility, agglutinating the organisms and neutralizing their exotoxins and then assist in their harmless elimination from the body in the fecal flow.
The concentration of sIgA gives us information about the intestinal immune defense:
A lack of sIgA indicates a diminished activity of the intestinal immune system.
An increase level of sIgA shows intestinal inflammation.
Beta-Defensin-2 ELISA test in stool samples
Defensins exert a variable degree of antimicrobial activity against bacteria, fungi, and some enveloped viruses. The expression of ß-defensins is induced by the pro-inflammatory cytokines and also through microorganisms (e.g. E. coli, H. pylori or P. aeruginosa) and by probiotic microorganisms. A ß-defensin-2 deficiency can, for example, be observed in the intestinal mucous of patients with Crohn’s disease. The defense system of the mucous membrane is therefore restricted and allows an increased invasion of bacteria, which could possibly lead to a typical infection in Crohn’s disease patients.
Recent results imply that ß-defensin-2 is overexpressed in active intestinal inflammation especially in ulcerative colitis.
EDN / EPX ELISA test in stool samples
The accumulation of EDN in the intestine is associated with inflammation and the tissue damage. Fecal EDN is considered the best of the cytotoxic granule proteins for assessment of gut inflammation. Elevated levels of fecal EDN are linked to multiple inflammatory conditions, like food allergy/sensitivity, pathogenic infections (C. difficile and H. Pylori), IBS, Eosinophilic Gastrointestinal Disorders.


Inflammation markers in stool samples
Hemoglobin : discharged with the feces in gastrointestinal bleeding diseases
Transferrin: a blood-derived component ; a good marker for gastrointestinal bleeding
Calprotectin: a neutrophil cytosolic protein with antimicrobial properties, which is present at increased concentration in stool during bowel inflammation.
Lactoferrin: a primary component of the acute inflammatory response released from fecal leukocytes; may serve as marker of inflammation in the intestine.
Assays for intestinal infections

FRÉMONT ET AL., IN VIVO 2009
INFECTIONS – assessment in stool samples
Ag-based testing for Clostridium, Yersinia, Enterovirus, Parasites, etc
INFECTIONS – PCR-based viral and bacterial assessment in intestinal biopsies
Stool-based assays for intestinal dysfunctions

ZONULIN ELISA test in stool samples
Zonulin is the “doorway” to leaky gut. Zonulin opens up the spaces between the cells of the intestinal lining. When leaky gut is present, the spaces between the cells open up too much allowing larger protein molecules and bacteria to get into the bloodstream where an immunologic reaction can take place. As the zonulin level rises, the seal between the intestinal cells diminishes. Zonulin is the only physiological modulator of intercellular tight junctions described so far that is involved in trafficking of macromolecules and, therefore, in tolerance/immune response balance.
MSA – Metagenomic Stool Assay
Until recently research into microbiota composition relied almost exclusively on culture ; 40 to 80% of gut bacteria cannot be cultured
Identification of colonies can be difficult
Bacteria must be alive: studies of anaerobes very difficult, major loss during collection and processing of samples
Culture approach may address only a small fraction of all bacterial species (10%?)
E.coli once thought to be a dominant species, is a minor member…
R.E.D. Labs scientists have developed and validated a new procedure to analyze bacterial populations in a stool sample : MSA assay
New molecular technique involving sequencing of specific regions of bacterial DNA (metagenomics)
Can be performed on dead organisms (exposure to oxygen, freezing are not a problem)
Identification of each bacteria by comparing sequence with public databases: extremely precise, not subjective
High-throughput technology allows identification of tens or even hundreds of thousends organisms in a single sample
Bacterial DNA was extracted from stool samples, PCR amplification was performed on 16S rRNA gene regions, and PCR amplicons were sequenced Bacteria were classified by phylum, family and genus.

Dysbiosis testing- msa test


Prevotella: strong hydrogen sulfide (H2S) producers. In excess, H2S acts as a mitochondrial poison and a potent neurotoxin. It can directly inhibit enzymes involved in the cellular production of energy. H2S also interferes with oxygen transport by blocking hemoglobin in the red blood cells. Finally, H2S is lowering gut pH preventing the growth of many beneficial bacteria (like Bifido).
Integrative approach for tbi part 3 – immune dysfunctions in tbd

MASON ET AL., TRENDS IN PARASITOLOGY 2013; DOI:HTTPS://DOI.ORG/10.1016/J.PT.2013.12.003
Immune dysfunction in tbd

Immune dysfunction in TBD
A hallmark of chronic Lyme disease is an underlying immune dysfunction that not only limits the ability to accurately diagnose Lyme, leaving many such patients misdiagnosed, but also serves as a major reason for lack of treatment response to antibiotics with an inability to eradicate the chronic infection.
The Borrelia bacteria (cause of Lyme disease) transforms from an acute to a chronic infection by transforming the body to a TH2 “extracellular” dominant response and then converting from a free swimming spirochete form in the blood into an intracellular form (L-form) to escape the elevated TH2 immunity. The suppressed and down-regulated TH1 intracellular immune response becomes an ineffective immune response by the body and an effective evasion strategy, which is the hallmark of transformation to late-stage Lyme dissemination.
Appropriate immune modulating therapies that are able to restore normal functioning immunity may be the biggest necessary leap forward in the development of an effective treatment protocol for this multi-system illness.
TH1/TH2 Balance
Th1/Th2 balance urine-based Th1/Th2 balance test
may detect disturbances of this delicate equilibrium in time in order to restore balance whenever required and before irreversible conditions are developing
allows patients to follow-up on Th1/Th2 balance during therapy (anti- oxydants, probiotics, nutraceuticals).


Testing for immune and metabolic dysfunctions

The extent of the global immune and / or metabolic dysfunctions could be evaluated by testing:
cytokine expression
elastase and perforin mRNA expression
oxidative stress, heavy metals, molds
macrophage phagocytic activity
alpha-N-acetylgalactosaminidase activity(Nagalase testing)
sCD14 expression
C3a & C4a expression
CD57 cell subset absolute count
prostaglandine E2 (PGE2) synthesis and hsCRP
VEGFsynthesis
ammoniaaccumulation
kynurenic and quinolinic acid accumulation, and many more
Testing for immune dysfunctions
The extent of the global immune dysfunction is evaluated by testing:
(1) cytokine expression
Testing for Th1/Th2 balance.
Testing for pro-inflammatory cytokines


The extent of the global immune dysfunction is evaluated by testing:
(2) elastase mRNA expression : a marker of inflammation
Elastase is an inflammatory protease expressed in immune cells (monocytes, neutrophils) that contributes to immune defense by inactivating foreign bacteria but at the same time it causes damage to connective tissue, breaks down cytokines, immunoglobulins and immune cells receptors. An excess, chronic production of elastase is therefore detrimental.Testing for Th1/Th2 balance.
(3) perforin mRNA expression : a mean to evaluate NK cell activation
Since NK cells play a central role in the defense against bacteria and viruses, decreased NK activity can lead to the development of opportunistic infections. NK cells exert their cytotoxic effect by releasing perforin, a protein that will destroy the cytoplasmic membrane of target cells and finally kill them.
The extent of the global immune dysfunction is evaluated by testing:
(2) elastase mRNA expression : a marker of inflammation
Elastase is an inflammatory protease expressed in immune cells (monocytes, neutrophils) that contributes to immune defense by inactivating foreign bacteria but at the same time it causes damage to connective tissue, breaks down cytokines, immunoglobulins and immune cells receptors. An excess, chronic production of elastase is therefore detrimental.
(3) perforin mRNA expression : a mean to evaluate NK cell activation
Since NK cells play a central role in the defense against bacteria and viruses, decreased NK activity can lead to the development of opportunistic infections. NK cells exert their cytotoxic effect by releasing perforin, a protein that will destroy the cytoplasmic membrane of target cells and finally kill them.


The extent of the global immune dysfunction is evaluated by testing:
(4) CD57 cell subset absolute count
CD57+/CD3- cells are a subset of NK cells. Their exact function, and what differentiates them from CD56+ NK cells, is not well understood. The absolute number of CD57+/CD3- cells is low in patients suffering from chronic Lyme disease (a disease that follows an infection by a bacteria called Borrelia). Patients with very low CD57 have significantly more co-infections and persistent immunologic defects than patients with higher counts. In patients that respond to antibiotic therapy, the number of cells come back to normal, hence this is a useful marker to follow the effect of a therapy.
(5) sCD14 expression
CD14 is expressed in monocytes/macrophages and plays a critical role in the recognition of bacterial cell wall components (LPS). The extracellular part of CD14 can be cleaved and released in the plasma, where it will inactivate circulating LPS. Serum soluble CD14 levels are significantly elevated in patients with inflammatory bowel disease, Crohn’s disease, but also in patients suffering from Brucellosis or Lyme disease.
The extent of the global immune dysfunction is evaluated by testing:
(6) C4A expression
C4a is an anaphylatoxin generated by cleavage of complement component 4 (C4), upon activation of the complement system. C4a increase causes local inflammatory response and symptoms of hypersensitivity. US study has reported that elevated complement C4a was an early marker for Lyme disease in tick bite patients. But C4A levels are decreased in chronic/late TBD patients
(7) prostaglandin E2 (PGE2) synthesis
(8) VEGF synthesis
(9) CD38 quantification

Pge2 production during illness and psychological stress

Quantification
FURUYASHIKI, T. & NARUMIYA, S. (2010) STRESS RESPONSES: THE CONTRIBUTION OF PROSTAGLANDIN E2 AND ITS RECEPTORS NAT. REV. ENDOCRINOL. DOI:10.1038/NRENDO.2010.194
Prostaglandine e2

Prostaglandin e2 (PGE2) synthesis
PGE2 is a compound derived from membrane phospholipids
PGE2 is also a key mediator of immunopathology in chronic infections and
cancer
PGE2 enhances its own production but suppresses acute inflammatory mediators, resulting in its predominance at late/chronic stages of immunity.
PGE2 selectively suppresses effector functions of macrophages and neutrophils and the Th1-, CTL-, and NK cell-mediated type 1 immunity, but it promotes Th2, Th17, and regulatory T cell responses.
PGE2 modulates chemokine production, inhibiting the attraction of proinflammatory cells while enhancing local accumulation of regulatory T cells and myeloid-derived suppressor cells.
Kynurenic and quinolonic acids


High levels of kynurenic acid have been identified in patients suffering from tick-borne encephalitis, schizophrenia and HIV-related illnesses. In all these situations increased levels were associated with confusion and psychotic symptoms
QUINO acts as a neurotoxin, gliotoxin, proinflammatory mediator, prooxidant molecule and can alter the integrity and cohesion of the blood–brain barrier. Quinolinic acid levels are increased in the brains of children infected with a range of bacterial infections of the central nervous system (CNS), in patients with poliovirus, Lyme disease with CNS involvement, traumatic CNS injury, hyperammonaemia, hypoglycaemia patie2n3 ts, systemic lupus erythematosus, malaria, etc.
VEGF
VEGF has a great role in pathological conditions that are associated to autoimmune diseases such as in systemic lupus erythematosus, rheumatoid arthritis, and multiple sclerosis.
Serum levels of VEGF correlate with disease activity in a large number of autoimmune diseases and fall with the use of standard therapy
Possible future therapeutic strategies in autoimmune diseases with the anti-VEGF or anti-VEGFR (receptor). So far, this therapy has been used in cancer and macular ocular degeneration in diabetes.
Abnormally high levels of VEGF in a mold-free environment would suggest Bartonella infection.
VEGF can go down in the presence of indoor molds.


CD38 IN TBD
CD38 in TBD (Hartiala et al. 2007, 2010)
CD38, which has an important role in dendritic cells (DC) chemotaxis and migration to lymph nodes, was strongly up-regulated by LPS of Gram – bacterias but practically not at all by Borrelia garinii (mostly inducing neuroborreliosis).
Borrelia garinii may affect crucial DC functions by blocking the up-regulation of important molecules in DC migration to lymph nodes, thus affecting further immune responses in Lyme borreliosis infection (Hartiala et al. 2007, 2010).
B. burgdorferi sensu stricto and B. afzelii are also unable to induce CD38 upregulation.
Thus low levels of CD38 might indicate Borrelia infection, while high levels of CD38 might indicate other Gram- infections and/or leaky gut
CD38 IN LYME

From Peacock et al. Redox Biology 2015
Focus on CIRS
CIRS = Chronic Inflammatory Response Syndrome
Ritchie Shoemaker: Pioneer in CIRS, Mold & Biotoxins
Body acquires biotoxins or toxin-producing organisms from foo, water, air or bug bites
Biotoxins cause continuing, unregulated production of cytokines
Multiple damages to the body with inflammation-related symptoms, immune system symptoms, resistant bacteria, chronic pain, sleep disturbance, gastrointestinal problems,….
Investigation of several markers from Shoemaker biotoxin pathway


VEGF
Cytokines
C3A & C4A
VIP & a-MSH
MMP-9
MARCoNS
Gastrointestinal problems
Altered hormone production
Vicious circle

Consequences of TBI

Remember
It is important to bear in mind that TBD can be acute or late stage / persistent / chronic; this is important given the testing and treatment approaches might be different in these two situations.
Lyme disease exhibits a variety of symptoms that may be confused with immune and inflammatory disorders.
If an individual has any chronic health condition, ranging from arthritis to chronic fatigue syndrome to fibromyalgia, it is important to rule out or diagnose Lyme disease. It is apparent that many cases of fibromyalgia and chronic fatigue syndrome are actually Lyme disease in disguise
In order to offer better management of patients with late/chronic and/or persistent infections that are very difficult to uncover, it is important to focus on an integrative approach, inclusive of direct pathogen detection as well as indirect supportive tests focusing on immune and gastrointestinal disorders.
Chronic patients have complex clinical picture with multiple afflictions needing thus multiple testing and careful interpretation of testing results.
Conclusions : integrative approach for tick-borne diseases testing
In order to offer better management of patients with chronic and/or persistent infections that are very difficult to uncover, focus both on direct pathogen detection as well as on indirect supportive tests (assessing immune and gastrointestinal disorders).
Direct tests for Persistent and/or chronic infections
Phelix phage borrelia test
Immunoblot for Borrelias, Chlamydias (pneumoniae, trachomatis, psittacii), Yersinia, EBV, Parvovirus, Treponema
Serology tests for CMV, Toxoplasmosis, Tularemia, Leptospira, BrucellaCapt
FISH test for Babesia
PCRs for Mycoplasma spp, Mycoplasma fermentans, Mycoplasma pneumoniae, Bartonella, Brucella, Coxiella, Babesia, Anaplasma, Ehrlichia, Chlamydias, Rickettsias, Midichloria mitochondrii, etc
PCRs for viral infections: herpesviruses like HHV-6, HHV-7, HHV-8, Parvovirus, EBV, TBE, etc
Testing for parasites, molds, etc
New tests


Indirect tests for Persistent and/or chronic infections
CD57 cell subset absolute count
CD38 quantification
cytokines’ expression, Th1/Th2 balance
sCD14 expression
prostaglandin E2 (PGE2) synthesis, VEGF, C4A and C3A quantification; KYNA & QUINO
Perforin and Elastase
Metal poisoning evaluation
Special focus on gastrointestinal disorders (dysbiosis, leaky gut, intestinal infections and inflammation, etc)
R.E.D. Laboratories who we are

R.E.D. Laboratories is Belgian company developing tests for chronic immune diseases and intestinal dysfunctions
We are involved in several international groups aiming to advance knowledge in biological markers of autism.
At R.E.D. Laboratories, we are continuously developing new tests according to the specific needs from health care providers.
All generated benefits are used for research and development of new assays.
Questions and contacts
References:
Material available on the website (www.redlabs.com)
Check regularly our website (www.redlabs.com) for the updates
Questions and contact:
Generalqueries,logistics: E-mailtoinfo@redlabs.be – Scientificquestions: E-mailtotmijatovic@redlabs.be